Bariatric Surgery
HomeIntroduction
- This recipe uses Total Intravenous Anaesthesia (TIVA) TCI.
- The main ingredients are Propofol and Remifentanil.
- Safe anaesthetic management and good postoperative analgesia is our goal.
- Patient weight, airway management and OSA have rarely caused anaesthetic issues.
- Although patients are well motivated and walk to operating theatre, those with bad arthritis and difficult mobility should be offered a wheelchair (or a bed).
- Reconfirm HDU bed if deemed necessary and don’t start the case unless it is available.
- Venous access could be difficult in few but often it is not a problem, we suggest 2 accesses.
- Measurement of blood pressure on the forearm with a normal arm cuff is all you need.
- Preexisting pressure effects on skin should be documented.
- Early postoperative mobilisation should be emphasised to avoid postoperative complications.
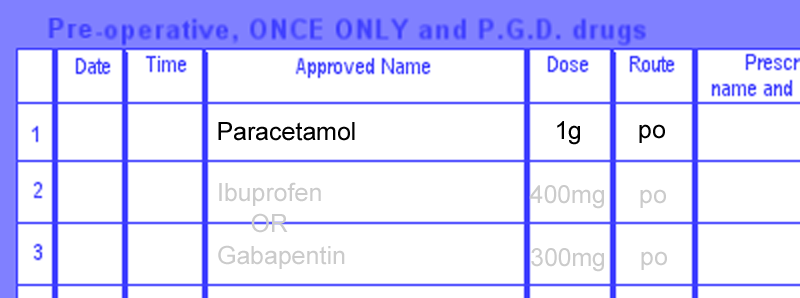
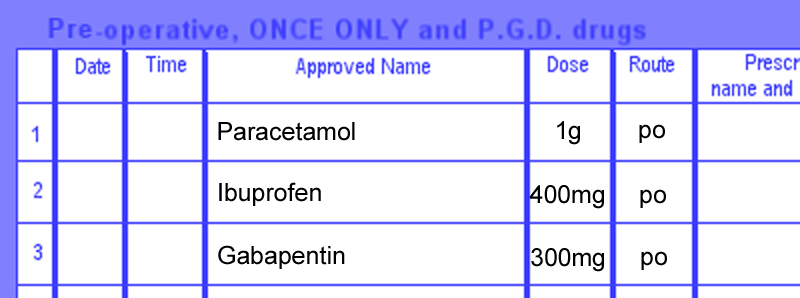
- Prescribe 2g of Paracetamol ± 400mg Ibuprofen ± PPI and other premeds in SAL.
.png)
Preparation
- Always get ready before your patient has arrived in theatre.
- Never get distracted when preparing anaesthetics and setting the infusions.
- Know your patient’s parameters (weight / age / height / sex / BMI) in advance to save time.
- Draw Propofol 2% in two 50ml syringes (you will need the second one sooner than you thought) and maybe a third one.
- Reconstitute 2mg of Remifentanil in 40mls of saline/water for injection (=50mcg/ml)
- Draw 2 vials of Rocuronium (10mls=100mg) as you will need more than just one dose. Always have Suxamethonium 200mg drawn and ready.
- Administer 4-8mg Ondansetron before induction and 3.3-6.6mg Dexamethasone after induction (to avoid perineal pain/heat).
- Get 20mg of Morphine drawn.
- Get 10mg of Metaraminol and 30mg Ephedrine drawn separately.
Setting the TCI Pump
- Use Propofol and Remifentanil in 2 separate pumps.
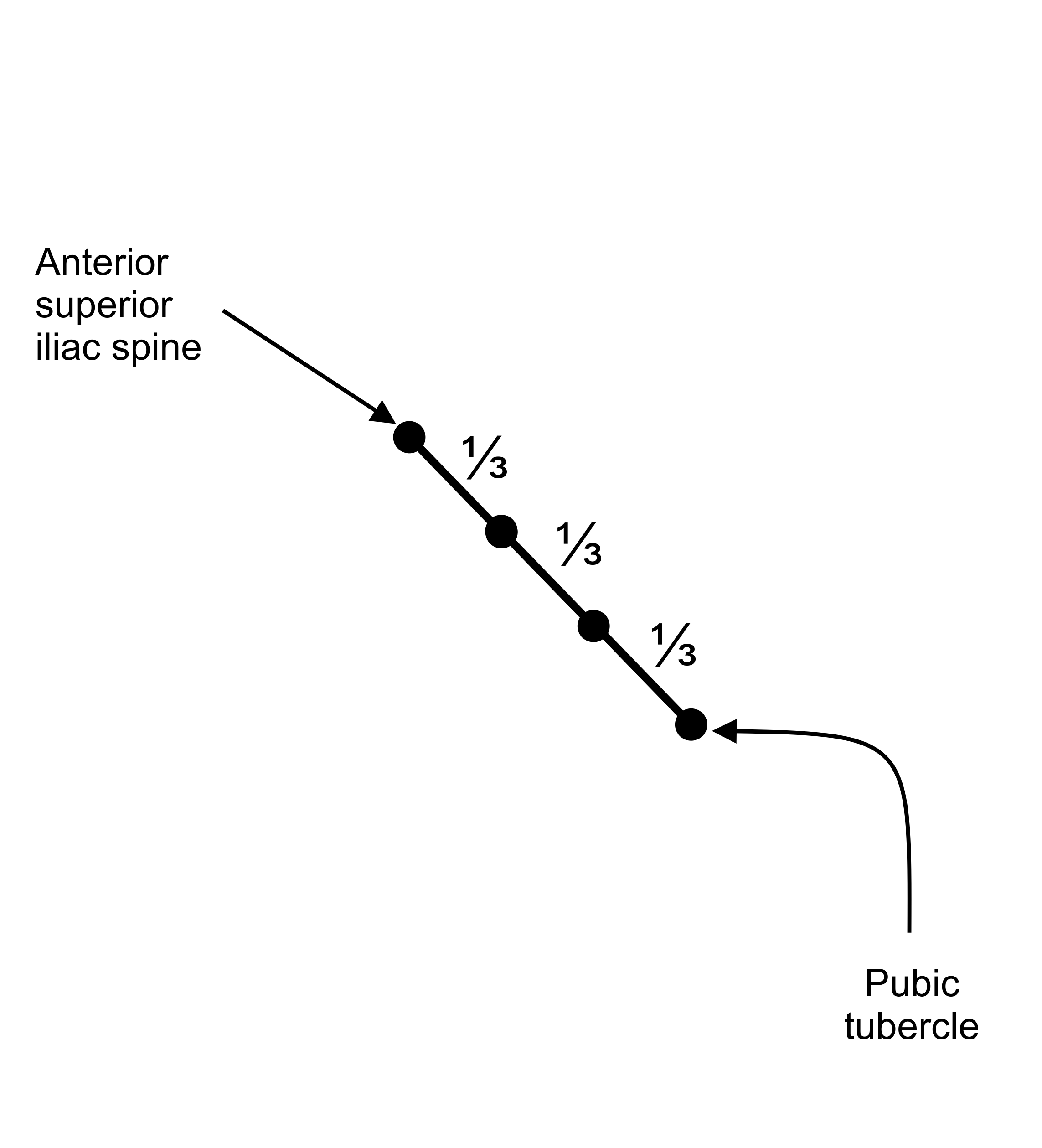
- How to calculate the Adjusted Body Weight for the TCI
-
Men: Height cm – 100 = Ideal Body Weight Women: Height cm – 105 - Extra Body Weight is the Actual Body Weight – Ideal Body Weight
- The Adjusted Body Weight is Ideal Body Weight + 1/3 Extra Body Weight.
- Example
-
If Mr.
Lone weighs 148
kg and is
168cm tall then
his Ideal Body Weight will be:
168 –
100 =
68kg,
IBW♂ = ht - 100, IBW♀ = ht - 105
-
Thus he weighs 80kg (Extra Body Weight) more than he should.
EBW = weight - IBW
-
His Adjusted Body Weight will then be:
68 +
27 =
95kg.
ABW = IBW + ⅓ x EBW
-
Meanwhile your patient has arrived.
- Help ID Check and positioning the patient on the table.
- The patient should sit first, then put feet on the foot rest before stretching up towards the pillow.
- The reverse Trendelenburg position makes the airway easier.
- Once patient is positioned, ask if there is any need of readjustment.
- The table has the Hover Mattress under the sheet, so there is a risk of patient sliding down if knees are bent or feet off the rest.
- Consider using Awareness Monitors and Arterial lines in difficult cases
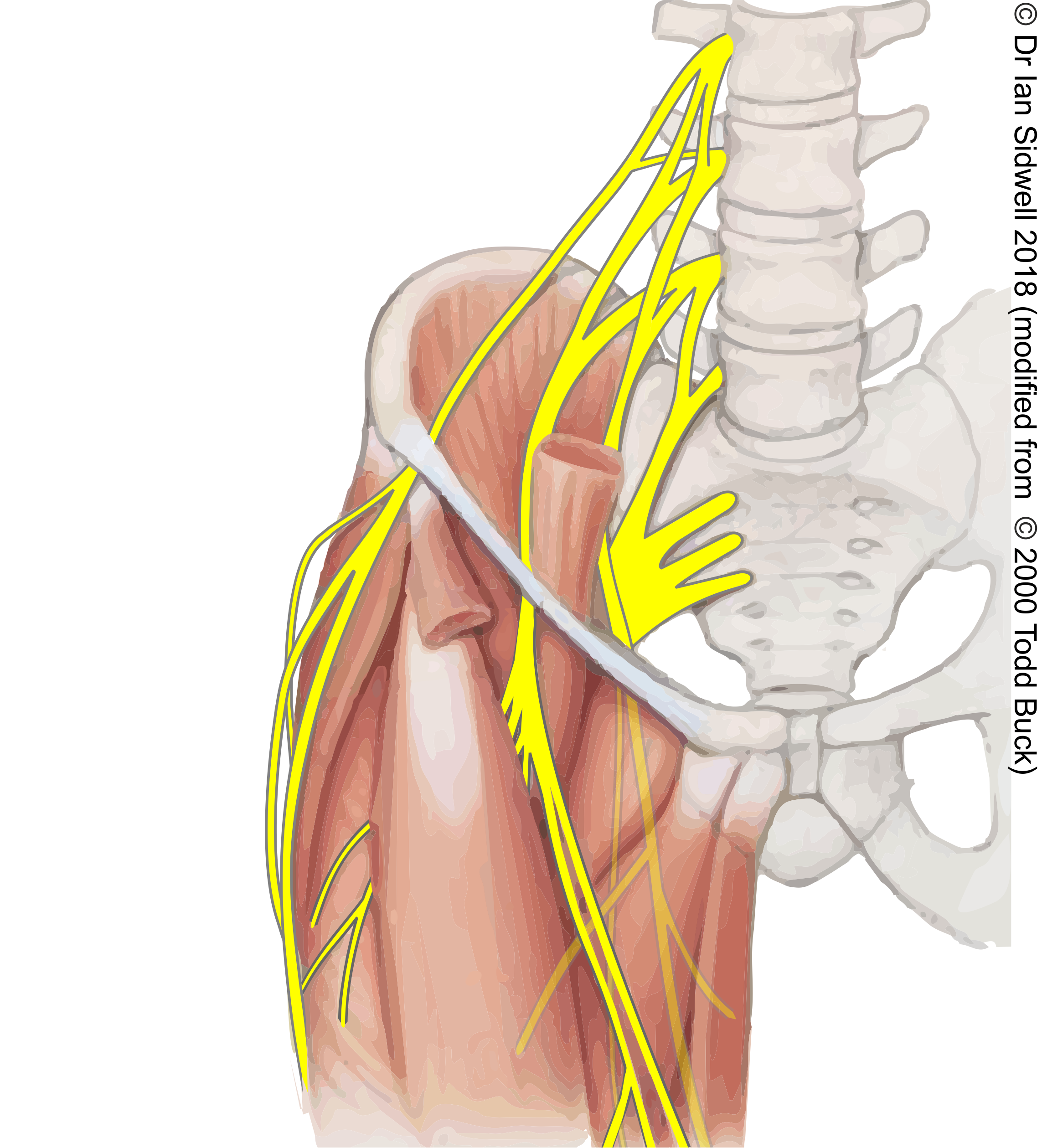
- This diagram will help patients to understand and anaesthetist to plan

- Welcome your patient
- Check the ID band
- Always position patient’s feet on the feet rest
- IV access / monitors
- Antibiotics/Antiemetics
- Preoxygenate/Flowtrons
- Induction/NMB/Intubation
- No BMV
Getting Ready for Take-off
- Put a 20-18G IV access in the arm away from the surgical instruments (monitors, cautery and suction) as the crowd will limit your IV access.
- Putting Flowtrons on before patient is asleep gives a feeling of good caring.
- Use normal BP cuff (blue) on the FOREARM near the surgical monitors.
- Record basic measurements before your patient is asleep.
- Administration of antibiotics and antiemetic before your patient is asleep gives the patient a feeling of care and buys you time for a final check: give them while preoxygenating (3 min), it saves time.
- Start FIRST the Remifentanil …target at 4-7nanogram (Minto).
- Once the Remifentanil has reached the target, start the Propofol at 5--7 microgram (Marsh): this makes intubation possible earlier and smoother.
- Administer the NMB once both Propofol and Remi have reached the targets.
- After one minute of NMB laryngoscope and intubate (avoid BMV).
- Once safely intubated, level the table to help the surgical team.
- Reduce the infusion rate by 1-2 nano/micrograms on both pumps until a minute before knife to skin as it helps to recover the drop of bp.
- Increase the infusion by couple of nano/micrograms if bp allows one minute before KTS.
- If KTS tolerated, reduce the TCI infusion.
- Always keep the Remifentanil infusion 1- 2 nanograms above the Propofol microgram as it helps CV and respiratory stability.
- If you have done BMV, the surgeon may ask to deflate the stomach. Use orally a big bore NG tube, make sure you remove it before the gastric part of the procedure commences.
- The table will be as low as possible with a side tilt so mind your IV line.
While Cruising…
- Avoid too much IV fluid, as blood loss will be amazingly low.
- Get oesophageal bougie and blue dye ready for bypass procedures.
- Dilute 10mls Methylene Blue in 150 to 250 mls of distilled Water.
- Fill the dye in two 50 mls bladder syringes to avoid accidental spillage.
- Get some KY Jelly ready.
- Before you are asked to put the bougie in, make sure you have topped up your NMB otherwise patient will cough.
- Watch the tip of your bougie arriving in on the surgeon’s monitor.
- Before taking it out, gently roll it between your fingers to “make sure it is not accidentally sutured”, Don’t just pull it out”.
- After the bougie is out insert the NG tube orally and watch on the screen for its tip arriving near the anastomosis.
- Before you inject the dye, make sure the ETT cuff is not leaky.
- Don’t force hard the dye syringe nozzle into the NG tube as you will then struggle to disconnect it if a second dye syringe is needed. Keep the second syringe handy to enhance the filling test/leak test if needed.
- Leave the suction ON inside the patient’s mouth before injecting the dye to avoid regurgitation on the pillow and patient’s face.
- By now you should have administered 2-3 doses of Morphine (5+5+5mgs) at good intervals.
- If Paracetamol was missed on SAL, this is the time to administer it IV.
- After the dye test you are left with 45 minutes to land so get your postop advice documentation and drug chart ready.
Getting Ready for Landing
- Always reverse NMB drugs to avoid any residual block.
- Stop Remifentanil once the abdominal ports are out, and reduce Propofol to half the maintenance infusion rate (2 microgram or less).
- Doxapram works well to stimulate respiration in case breathing is slow.
- Make sure your surgeon uses local anaesthetics (40ml bupivacine 0.25% or L-bupivacaine) around the port sites.
- Extubate (sat up) once respiration and SpO2 acceptable (consider a Guedel).
- Before sliding on to the bed make sure Hover mattress loops are free on all sides.
- As the patient needs to be sat up, transfer the patient towards the head end of the bed, otherwise patient slips down south once sat up (see diagram).
You Landed
- Prescribe IV Morphine
- Prescribe an antiemetic for use in the recovery and ward.
- Prescribe oral analgesia for ward (Oromorph/Paracetamol/Tramadol). IV rarely needed.
- Make sure patient on CPAP has his machine available on the ward.
.png)
.png)
.png)
Notes
- A Gastric Bypass usually takes more than 2 hours and Gastric band less than two hours.
- A Gastric Band patient is likely to be sent home same day, so “Consider Fentanyl Analgesia” in PACU.
- These patients will need an hour in the recovery to get fit for transfer to ward.
- Always See your patient and recovery staff before they are transferred.
- Make sure you complete the documents before your patient is transferred to the ward.
References
- Anaesthesia for the Overweight and Obese Patient by M Bellamy and M Struys (Oxford University Press 2007 ISBN-13:9780199233953)
- An overview of TCI & TIVA by A Absolam and M Struys (Academia Press, 2007 ISBN-13 9789038211077)
- Lecture Notes: M Bellamy, M Margarson (Recent Advances in Anaesthesia, Critical Care and Pain Management 2-4 Feb 2011, Pages 103-7)
- Designing intelligent anesthesia for a changing patient demographic: a consensus statement to provide guidance for specialist and non-specialist anesthetists written by members of and endorsed by the Society for Obesity and Bariatric Anaesthesia (SOBA) Bellamy and Margason - Perioperative Medicine 2013, 2:12 http://www.perioperativemedicinejournal.com/content/2/1/12
- Peri-operative Management of the Morbidly Obese Patient - AAGBI 2007 www.aagbi.org/sites/default/files/Obesity07.pdf
- My personal experience over the past ten years of more than 100 patients at MPH Taunton
- SOBA guideline
Acknowledgments
- Prepared by Mohammad Lone for use by occasional bariatric anaesthetic colleagues